What is OCD?

Have you ever heard someone say (or said it yourself), “I’m so OCD.”?
What does that even mean?
Most people have obsessive thoughts and/or compulsive behaviors at some point in their lives,
but that does not mean that we all have “some OCD.”
How do I know if I have OCD?
Obsessive Compulsive Disorder (OCD) is a mental health disorder that is diagnosed by a trained mental health professional using observation & assessment (there are no definitive medical tests), and is characterized by:
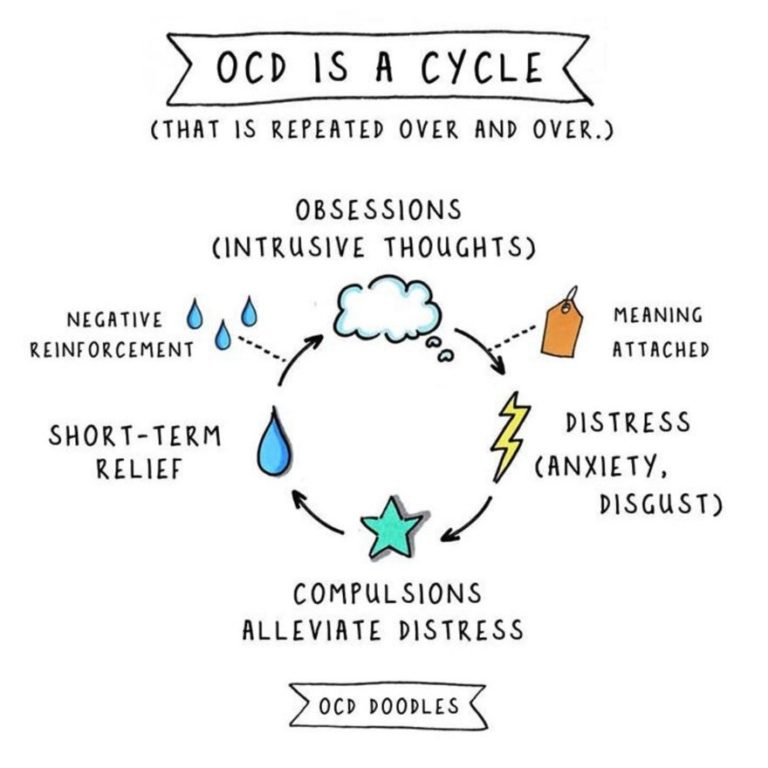
1) distressing thoughts (obsessions) – unwanted, intrusive thoughts. These types of thoughts may present themselves as ideas, images, urges, memories, or other information and trigger intensely distressing feelings.
2) repetitive behaviors or mental acts (compulsions) – behaviors that are designed to reduce or avoid the discomfort that comes from the obsessions, that;
3) interfere with your life, are time-consuming, and are very difficult to control.
OCD Cycle
For example, if you’re afraid
of contamination, you might develop elaborate cleaning rituals. However, the relief never lasts. In fact, the obsessive thoughts usually
come back stronger. And the compulsive behaviors often end up causing anxiety themselves as they become more time-consuming, leading to impaired functioning and a reduced quality of life. This is the vicious cycle of OCD.
How common is OCD?
Studies show that OCD lifetime prevalence rate is estimated at between 2 and 3% (about 1 in 40). This is even higher when you include people with “subclinical” symptoms – as high as 28% of a large US sample report experiencing obsessions or compulsions at some point during their life. OCD definitely runs in families – there is an up to five times increase in occurrence of OCD among 1st degree relatives (parents, children, siblings).
When does it typically begin?
OCD can start as young as preschool age, but young adults between ages 18 and 24 are at the highest risk for developing OCD. Onset in males is typical, in their late teens. For females onset is typically in their early twenties. Developing OCD after age 30 is rare.
What causes OCD?
While the exact cause is not known, it is thought to be a combination of genetics, environment, and psychological factors (e.g. childhood adversity, stressful life events, past learning). Research has shown that people with OCD are not able to simply turn off their obsessive thinking – their brains are wired differently than people without OCD. A simplified explanation of the frontostriatal model (formulated by Pauls et al, 2014) describes possible abnormalities of certain neurotransmitter systems (serotonin, dopamine & glutamate):
“When danger is sensed, the brain switches on a warning light. Usually the warning light would be switched off after it has confirmed there is in fact no danger. However, in OCD, the process for switching off the warning light does not work as effectively as it should, leaving you with a lingering sense of danger and a feeling that you need to do more to make the situation safe, despite there being no realistic need for that”.
How is OCD treated?
Contacting a properly trained therapist is a good place to start. That person will be able to confirm the diagnosis, help you develop a treatment plan, and support & guide you along the path to obtaining relief from your symptoms.
Exposure and response prevention (ERP) therapy is one of the most effective forms of treatment for OCD. ERP therapy will help to gradually reduce your anxieties so you can stop the cycle of OCD. An important part of how this is done is to help you avoid the compulsions. You basically learn that your distress and uncertainty about what will happen can be tolerated. This can seem like a big, frightening change, so therapists usually start with low to moderately anxiety-provoking exposures and work their way up to higher-level exposures. Read more about ERP
Your therapist will also discuss the possibility of using medication in conjunction with therapy. Antidepressant medications, especially the SSRI class (newer) have been shown to be quite helpful, most likely because they increase the effects in the brain of the neurotransmitter serotonin. Your therapist can help you connect with an appropriate medication prescriber.
Family support & education is also an important part of effective help for your OCD. Family members are very affected by OCD. Family Accommodation Behaviors are things families do that enable OCD symptoms. Research shows that how a family responds to the OCD may help fuel OCD symptoms. The more that family members can learn about their responses to OCD and the impact they have on the person with OCD, the more they are able to help their loved one relieve their OCD symptoms.
What are the obstacles to treatment?
It takes an average of 14-17 years to obtain appropriate treatment. This is due to: stigma/embarrassment; lack of public awareness; lack of understanding by some mental health professionals; difficulty finding local therapists who can effectively treat OCD
What is the typical prognosis?
While there is no definitive cure for OCD, you can greatly influence how long it takes to benefit from treatment. The more consistent that you are in attending therapy sessions and the more homework assignments that you complete on your own, the faster you will see results. This change may not be linear, but few things in life are, so stick with it!
Remember that getting well is only half the battle; you need to make sure that you take steps to stay well, too.
What should I look for in a therapist?
Your relationship with the therapist is important, especially since they will be asking you to do things that you find uncomfortable, so you have a perfect right to ask questions.
Some things to consider are: does the therapist have experience in treating OCD?; do they use ERP?; how much of their practice involves working with people with OCD?; are they are member of the International OCD Foundation (IOCDF)?; what are their thoughts about using medication (which can be quite helpful) along with ERP therapy?
Clark, D.A.. (2020). Cognitive-Behavioral Therapy for OCD and Its Subtypes . New York. Guilford Publications, Inc
Hershfield, J. & Corboy, T. (2013). The Mindfulness Workbook for OCD. Oakland, CA. New Harbinger Publications, Inc.
Obsessive-Compulsive and Related Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association.
https://www.helpguide.org/articles/anxiety/obssessive-compulsive-disorder-ocd.htm
International OCD Foundation retrieved: https://iocdf.org/about-ocd/
Van Niekerk, J. (2018). A Clinician’s Guide to Treating OCD: The Most Effective CBT Approaches for Obsessive-Compulsive Disorder. Oakland, CA. New Harbinger Publications, Inc.
